Goiter & Thyroid Nodules
Enlargement of the thyroid (goiter) and lumps within it (nodules) are both relatively common. They may be obvious to the naked eye or can be found incidentally by imaging studies of the neck, such as a sonogram of the carotid arteries or a CT or MR of the spine. Most goiters and thyroid nodules will not interfere with a person's health.
Overview
Goiters and thyroid nodules causing unwanted symptoms or adversely affect a person's health require treatment, often thyroid surgery. These situations include:
- Large goiters that are uncomfortable or cause breathing difficulties or swallowing.
- Multinodular goiters, particularly those that constrict airways, the esophagus or blood vessels.
- Thyroid nodules that have an indeterminate diagnosis or are deemed suspicious for cancer after biopsy.
- Nodular goiter causing hyperthyroidism (overactive thyroid) where treatment with radioactive iodine or anti-thyroid medications are not an option
- Goiters or nodules that are malignant (thyroid cancer)
A thyroidectomy is a surgical procedure to remove all (total thyroidectomy) or part of the thyroid gland (partial thyroidectomy). Patients may also need to take the drug levothyroxine, an oral synthetic thyroid hormone, after surgery dependent on the how much of the gland is removed.
What is a goiter?
Goiter refers to enlargement of the thyroid gland, a butterfly shaped organ draped around the front and sides of the windpipe (or trachea) in the lower part of the neck.
The thyroid gland is normally about the size of two thumbs held together in the shape of a V. It can enlarge when it is inefficient in making thyroid hormones, inflamed, or occupied by tumors.
Thyroid gland enlargement can be generalized and smooth, a so called diffuse goiter; or it can become larger due to growth of one or more discrete lumps (nodules) within the gland, a nodular goiter.
A goitrous gland can continue producing the proper amounts of thyroid hormones, in which case it is called a euthyroid or nontoxic goiter; or a goiter can develop in conditions with either overproduction of thyroid hormone, called toxic goiter, or the inability to make sufficient thyroid hormones, called goitrous hypothyroidism.
What is a Thyroid Nodule?
A thyroid nodule is simply a lump or mass in the thyroid gland. Thyroid nodules are relatively common; 6% of adult women and 2% of adult men in the U.S. have a thyroid nodule that can be felt on examination. Moreover, close inspection of the thyroid by sonographic imaging shows that as many as one-third of women and one-fifth of men have small nodules in their glands.
The thyroid may contain just one nodule (solitary thyroid nodule or uninodular goiter) or several of them (multinodular goiter). Thyroid nodules can be solid if they are comprised of thyroid or other cells or an accumulation of stored thyroid hormone called colloid. When nodules contain fluid, they are called cystic nodules. These can be completely fluid filled (simple cysts), or partly solid and partly fluid, (complex cysts).
Thyroid nodules vary greatly in size. Many are large enough to see and feel (palpable nodules). Some multinodular goiters can become enormous, bulging out of the neck and over the collar bones or extending down into the chest behind the breastbone, a condition called substernal goiter. At the other end of the spectrum, the majority of thyroid nodules are too small to see or feel at all, and are called nonpalpable nodules.
Such small nodules are found when a person has a medical imaging procedure performed for some other reason, such as a sonogram of the carotid arteries; a CAT or MRI scan of their neck, head, or chest; or a PET scan. These very small, incidentally detected thyroid nodules are called thyroid incidentalomas.
Finally, of course, thyroid nodules can also be classified as benign or malignant depending on whether the cells of which they are comprised have the potential to spread beyond the thyroid gland into adjacent tissues or distant parts of the body. Specific causes of thyroid nodules and how they are distinguished are discussed below.
Multinodular Goiter
A multi-nodular goiter is an enlarged thyroid gland with a goiter comprised of multiple thyroid nodules. The nodules can be very small (often only a few millimeters in size) or a larger size (several centimeters) and there is often a dominant nodule. The key question is whether the nodules are benign or malignant (cancerous). This is discussed in more detail below.
What the Thyroid Gland Does
To understand why some types of goiter develop, it is first important to know what the normal function of the thyroid gland is and how it is regulated. The thyroid gland makes and releases into blood two small chemicals, called thyroid hormones: thyroxine (T4) and triiodothyronine (T3). Each of them is comprised of a pair of connected tyrosine amino acids to which four or three iodine molecules, respectively, are attached.
The iodine needed for thyroid hormone production comes from our diet in seafood, dairy products, store bought bread, and iodized salt. Once absorbed, iodine in blood is trapped by a special pump in thyroid cells, called the sodium-iodide symporter. The thyroid also has several specialized biochemical 'fastening machines,' called enzymes, that then carry out the steps needed to attach iodine to particular parts of a very big protein called thyroglobulin, which is made only by thyroid cells.
Some of this thyroglobulin with iodine molecules attached is stored in the gland in the form of a gooey paste called colloid, which is normally located in the center of follicles, which are balls of thyroid cells with a hollow center.
A regulated amount of the thyroid hormones is constantly being chopped off of thyroglobulin and secreted into blood for delivery to tissues throughout the body. In the nucleus of almost every cell, thyroid hormones bind to molecules called T3 receptors, which are attached to segments of DNA that regulate certain genes. Precise control of how many proteins are made from these genetic blueprints maintains the normal or euthyroid thyroid state. Excessive activation of these genes by abnormally high thyroid hormone levels causes hyperthyroidism; inadequate gene activation due to insufficient thyroid hormone production causes hypothyroidism.
The thyroid normally makes precisely the right amount of its hormones under the exacting control of the pituitary gland, which is an extension of the brain. Specialized pituitary cells make thyroid stimulating hormone (TSH), which travels in blood to the thyroid gland, where TSH binds to its own receptors on thyroid cells, prompting them to grow and produce more of the thyroid hormones. Normally, this system is kept in balance by the negative feedback of the thyroid hormones on TSH-secreting pituitary cells (as well as the part of the brain that controls them).
Causes of Goiter
Three categories of problems are responsible for almost all cases of thyroid gland enlargement: inefficient thyroid hormone production, gland inflammation, and tumors in the thyroid:
- When the gland is inefficient in making sufficient thyroid hormone, it compensates by getting bigger. Worldwide, the most common cause is dietary iodine deficiency, a condition estimated still to affect 100 million people who live in poverty-stricken societies. Iodine is an essential building block for thyroid hormones; in the absence of adequate supply, the gland becomes larger.
When more than 10% of a population has goiter due to iodine deficiency, it is called endemic goiter. Other consequences of severe iodine deficiency include hypothyroidism and cretinism, a syndrome of mental retardation, short stature, deafness, and characteristic facial deformities that affects children born to hypothyroid mothers in iodine deficient regions. (For more information, see the International Council for Iodine Deficiency Disorders website:www.iccidd.org.)
People with defects in their genetic blueprints for the proteins that permit the thyroid gland to make thyroid hormone (e.g., mutations in the molecular pump that enable the thyroid to concentrate iodine within itself) typically develop a goiter. Certain drugs can also interfere with normal thyroid function and lead to compensatory gland enlargement, such as lithium carbonate, which causes a goiter in 10% of individuals taking this medicine. - Inflammation of the thyroid gland (thyroiditis) can produce gland swelling. Some forms of thyroid inflammation are quite common, such as autoimmune thyroiditis and painless (postpartum) thyroiditis. Autoimmune thyroiditis (also called Hashimoto thyroiditis) occurs when a person's immune system turns against their own thyroid gland, inflaming it, usually causing the gland to swell, and often making it permanently underactive.
Autoimmune thyroiditis can first appear in children and young adults, but its incidence increases sharply in middle aged and elderly people. Other types of thyroiditis causing goiter include: 1. painless (postpartum) thyroiditis, a self-limited inflammation of the thyroid that can resolve without treatment and affects at least five per cent of women in the year after pregnancy; 2. subacute thyroiditis, which causes painful thyroid enlargement as the result of viral infection; and 3. other rarer forms of infectious thyroiditis; and 4. drug-induced thyroiditis, such as those caused by amiodarone and interferon alfa; and 5. a rare fibrosing condition called Reidel thyroiditis. (For more information, see Knol on Thyroiditis.) - Goiter can be the result of thyroid tumors, which are usually benign, but sometimes malignant. Most thyroid tumors present as discrete nodules, but there are several kinds of thyroid cancer that can cause generalized swelling of the gland. These include infiltrating papillary thyroid cancer, lymphoma, and anaplastic thyroid cancer. Certain facts make it important to consider the possibility that a goiter might be malignant.
These include one or more of the following symptoms: rapid enlargement of a goiter over a few weeks, the onset of new thyroid-related pain, difficulty swallowing, shortness of breath, or coughing up blood; or a goiter in someone with risk factors for thyroid cancer, such as a person who had childhood radiation to their neck or who has a close relative with thyroid cancer. (See below and the Knol on Thyroid Cancer.)
Table 1. Causes, Features, and Treatments for Certain Common Causes of Goiter
| Type of Goiter | Cause | Typical Symptoms and Signs |
|---|---|---|
| Iodine deficiency (endemic goiter) |
Lack of sufficient dietary iodine intake |
Thyroid gland enlargement (goiter) |
| Graves disease (diffuse toxic goiter) |
Autoimmune stimulation of the thyroid gland |
Goiter |
| Autoimmune thyroiditis (Hashimoto, chronic lymphocytic) | Persistent immune system inflammation of person's own thyroid |
Goiter |
| Subacute thyroiditis (painful, de Quervain) |
Viral infection |
Painful, tender and swollen gland |
| Toxic adenoma and toxic multinodular goiter | Benign thyroid tumor(s) |
Nodular goiter |
| Goiter and thyroid nodules suspicious for malignancy | Malignant thyroid tumors |
No symptoms |
Causes of Thyroid Nodules
Thyroid nodules, masses in the thyroid gland, can be the result of benign cell overgrowth (adenomatous hyperplasia) or actual discrete tumors comprised of thyroid cells that can be benign or cancerous. Thyroid nodules can sometimes contain fluid, which usually collects due to bleeding from the fragile blood vessels in thyroid tumors, so called cystic degeneration. This event sometimes causes the sudden onset of pain and swelling in the front of the neck, which typically subsides over several days.
Fortunately, more than 90% of thyroid nodules are not cancers, but malignancy should be considered in every affected person. Often patients with small thyroid nodules, less than 1 cm in diameter, and no risk factors for thyroid cancer can simply be reexamined or imaged by sonography to be sure the nodule is not enlarging. For larger nodules, additional studies are usually indicated, as described below.
Key Issues in Goiter & Thyroid Nodule
Whenever a person has a goiter or thyroid nodule, three questions must be answered.
- Is the gland, or a portion of it, so large that it is stretching, compressing, or invading nearby structures?
Thyroid swelling can cause a sensation of tightness or, less commonly, pain in the front of the neck. A goiter or nodule can compress the windpipe (trachea) causing cough or shortness of breath, while pressure on the swallowing tube (esophagus) can cause discomfort with swallowing or even the inability to get things down. When a goiter extends down into the chest, blood returning from the neck and head can be partially obstructed, causing neck veins to bulge. When a goiter or nodule is due to cancer, the tumor may actually grow into nearby structures, causing pain, hoarseness when nerves to the voice box are invaded, or coughing up blood when the trachea is penetrated.
- Is the gland functioning normally, or is it overactive or underactive?
Goiter is a characteristic feature of all the common forms of hyperthyroidism. For example, in hyperthyroid Graves disease, there is usually a diffuse or generalized goiter; and in toxic adenomas and toxic multinodular goiter, there are solitary and multiple nodules, respectively in the gland. Individuals with hyperthyroidism due to either painless thyroiditis or subacute thyroiditis also usually have a modest diffuse goiter.
Conversely, people with hypothyroidism also often have a goiter. For example, the most common cause of hypothyroidism, autoimmune thyroiditis, typically causes diffuse gland enlargement that is 1½ to 3-times normal size. Consequently, thyroid function must be assessed in all patients presenting with goiter or a thyroid nodule. The best single test to screen for both conditions is the serum thyroid stimulating hormone (TSH) concentration, which is suppressed to a low level in people with hyperthyroidism, and elevated in those with hypothyroidism. - Third, is the goiter or thyroid nodule due to malignancy? Fortunately, most patients with a goiter or thyroid nodule do not have thyroid cancer. Often other findings in a patient with a goiter, such as the features of hyperthyroid Graves disease, make it unnecessary to do additional tests to rule out cancer. On the other hand, almost everyone with a thyroid nodule larger than 1.0 to 1.5 cm in diameter must be investigated for the possibility of thyroid cancer. The approach to these diagnostic evaluations is discussed below.
Answering these three important questions begins with collecting certain facts about the person's medical history and any recent symptoms. (Table 2)
Table 2. Key Issues to Evaluate in a Person with a Goiter or Thyroid Nodule
|
Gender and Age
|
Goiter and nodules are more common in women and older people, but nodules in men and younger are somewhat more likely to be cancer |
|
Local Neck Symptoms
|
Swelling or pain in the front of the neck |
|
Symptoms of Possible Cancer Spread |
Bone pain in one spot without relief |
|
Hyperthyroid Symptoms
|
Weight loss, heat intolerance, trembling hands, palpitations, insomnia, anxiety, increased bowel movement frequency - especially if the symptoms are new or persistent |
|
Hypothyroid Symptoms
|
Weight gain, cold intolerance, constipation, very dry skin, slowed thinking, depressed mood, muscle cramps - especially if the symptoms are new or persistent |
|
Risk factors for thyroid cancer
|
Childhood neck radiation |
Diagnosis
A doctor will look on physical examination for signs related to the thyroid enlargement: the entire gland or nodule size; its firmness, mobility, and tenderness; and whether there is any nearby lymph node enlargement. The doctor will also look for signs of thyroid hormone excess or deficiency. Although the history and physical examination sometimes provide important clues, it is almost always necessary to perform additional diagnostic tests to answer the key clinical questions with certainty.
A thyroid sonogram beams inaudible sound waves into the neck and the returning echoes depict thyroid and surrounding tissues; this can confirm that a lump in the neck is in the thyroid gland, show whether it is cystic or solid, and precisely measure its size. A blood test for TSH can rule in or out all of the common causes of hyperthyroidism and hypothyroidism.
If the TSH is low, then there is a possibility the person has a benign, but hyperfunctioning thyroid adenoma; so the next step for these individuals is often a radionuclide thyroid scan to see if the gland enlargement is, in fact, a "hot" nodule. This is important, because almost all cancerous thyroid nodules are "cold" on radionuclide scanning; unfortunately, so are many benign thyroid nodules, so the test is not very helpful in people who do not already have a low TSH blood test suggesting hyperthyroidism.
If the TSH is elevated, the person probably has an underactive thyroid gland, and its enlargement may be a sign of autoimmune thyroiditis. If the TSH is normal or high, then most individuals with a thyroid nodule larger than 1.0 to 1.5 cm (1/2 inch) in diameter as well as those with a suspicious goiter need to have a fine needle aspiration biopsy to obtain thyroid cells for cytologic evaluation by an expert pathologist.
Thyroid biopsy results fall into four categories. ) First is an inadequate specimen in which there simply is not enough thyroid tissue to make a diagnosis. People with this finding need another biopsy.
Second, and fortunately, most often, the biopsy report is benign. People with this category of nodule usually need no surgery and can be seen by their doctor periodically to sure their goiter or nodule is not progressively enlarging.
Third, the biopsy can strongly suggest the presence of thyroid cancer. When the biopsy findings are malignant, 95% of the time, the person will actually prove to have thyroid cancer at subsequent surgery, so an operation is indicated unless the individual has other serious medical problems.
The fourth category of thyroid biopsy finding is uncertain or indeterminate. One in five biopsies fall into this group, in which adequate tissue has been obtained, but the features of the cells seen just are not characteristic enough of a benign or malignant nodule to be sure. Surgery is usually also indicated for this last group (see below), because among people with this biopsy outcome, 15% will prove to have thyroid cancer once the nodule is removed surgically and fully examined.
Treatment
Whether a goiter needs treatment depends on the answers to the three key clinical questions. If the thyroid is so large as to cause symptoms by stretching or compressing adjacent structures, or if it is so big as to be unsightly, surgical removal of the thyroid gland (thyroidectomy) may be required. If the goiter is related to a condition causing hyperthyroidism, as in Graves disease or toxic nodular goiter, treatment with radioactive iodine may be effective in both controlling gland overactivity and decreasing its size.
Some normally functioning (nontoxic) nodular goiters can also be shrunk with radioactive iodine therapy. If the thyroid is enlarged as the result of autoimmune (Hashimoto) thyroiditis and the gland is also underactive with a high blood TSH level, then starting thyroid hormone medication (L-thyroxine) may both treat the hypothyroidism and partially shrink the gland.
Surgery
Similarly, thyroid nodules may also require surgical removal or radioactive iodine based on their size and whether they are causing hyperthyroidism. In addition, thyroid nodules that are found to be suspicious for malignancy must be removed along with the remainder of the thyroid gland to prevent the spread of thyroid cancer.
Most people with a cytologically uncertain finding are also advised to have at least the half of their thyroid gland with the nodule removed because one in seven of these individuals will be found to have thyroid cancer. The use of thyroid hormone to put the thyroid gland to rest and shrink thyroid nodules-often prescribed in the past-has now been found to be relatively ineffective.
Benefits and Risks of Surgery
Thyroid surgery can remove one-half (thyroid lobectomy or hemi-thyroidectomy) or all of the thyroid gland (total thyroidectomy) to establish with certainty whether a goiter or nodule is cancer or not. Surgery to remove an enlarged thyroid can relieve compression of nearby structures and improve symptoms in patients with related difficulty swallowing, cough, or shortness of breath. Thyroid surgery can also cure certain forms of thyroid gland overactivity associated with goiter or nodules.
Thyroid surgery almost always requires hospitalization and anesthesia. The incision causes pain for a day or two after surgery, and it leaves a scar, which is usually relatively inapparent after a year. As with any operation, bleeding and infection can complicate thyroid surgery.
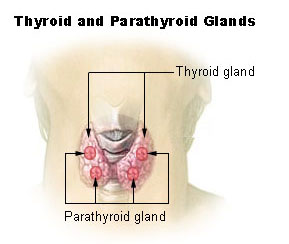
Behind the thyroid gland, there are two sets of important structures that can be accidentally injured during the course of a thyroid operation. The recurrent laryngeal nerves run along side the windpipe on their way to the voicebox (larynx), where they control the muscles that move the vocal cords. If one of these nerves is cut, smashed, or has its blood supply cut off, then a person will suffer some degree of voice loss.
This vocal cord paralysis can lead to a range of voice changes, ranging from losing a high octave or two while singing to the inability to shout to a severely disabling whisper of a voice. If both recurrent laryngeal nerves are injured, then a person may have difficulty breathing and require that a hole be created connecting the windpipe with the front of the neck (tracheostomy).
Four parathyroid glands are also located behind the thyroid: two on each side. If the parathyroids are accidentally removed or injured, then the patient's blood calcium levels drops-resulting in tingling, numbness, and muscle cramps. Rarely, a severely low calcium level can lead to throat spasm or a seizure. Fortunately, these complications are unusual in the hands of an experienced thyroid surgeon; mild injuries often resolve spontaneously over days or weeks after surgery; and there are treatments that can improve matters.
Radioactive Iodine
Radioactive iodine is mainly used for treated of a goiter or nodule when it is the cause of an overactive thyroid gland. Radioactive iodine is also sometimes used to shrink a goiter that is not overactive.
UCSF is a major referral center for endocrine surgery. Endocrine surgeons at UCSF perform a high volume of thyroid procedures with generally excellent results.




