Hemorrhoidectomy
A hemorrhoidectomy is surgery to remove internal or external hemorrhoids that are extensive or severe. Surgical hemorrhoidectomy is the most effective treatment for hemorrhoids, though it is associated with the greatest rate of complications.
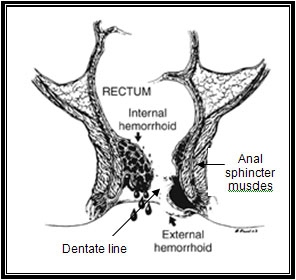
Hemorrhoid Anatomy
Illustration reprinted with permission from the American Society of Colon and Rectal Surgeons. Artist: Russell K. Pearl, M.D.
A hemorrhoidectomy is performed in the following settings:
- Symptomatic grade III, grade IV, or mixed internal and external hemorrhoids
- Where there are additional anorectal conditions that require surgery
- Strangulated internal hemorrhoids
- Some thrombosed external hemorrhoids
- Where patients who cannot tolerate or fail minimally invasive procedures
Types of hemorrhoidectomies and related procedures performed during surgery:
- Closed Hemorrhoidectomy
- Open Hemorrhoidectomy
- Stapled Hemorrhoidectomy (Procedure for Prolapse and Hemorrhoids - PPH)
- Rubber band Ligation
- Lateral Internal Sphincterotomy
Closed Hemorrhoidectomy
Closed hemorrhoidectomy is the surgical procedure most commonly used to treat internal hemorrhoids.
It consists of the excision of hemorrhoidal bundles using a sharp instrument, such as a scalpel, scissors, electrocautery, or even laser followed by complete wound closure with absorbable suture. Typically all three hemorrhoidal columns are treated at one time. Postoperative care includes frequent sitz baths, mild analgesics, and avoidance of constipation. Closed hemorrhoidectomy is successful 95% of the time.
Potential complications include pain, delayed bleeding, urinary retention/urinary tract infection, fecal impaction, and very rarely, infection, wound breakdown, fecal incontinence, and anal stricture. Although this technique has the most postoperative discomfort and pain, it does have the best long term results with the lowest recurrence rates. New methods are being devised to decrease the pain associated with the surgery and should allow for a better patient experience.
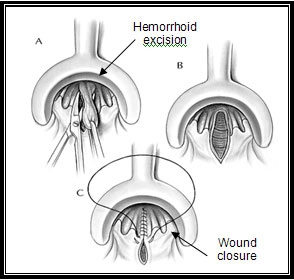
Closed Hemorrhoidectomy
Source: Hemorrhoids:By Andrea C. Bafford, M.D. and Ronald Bleday, M.D [Internet]. Version 20. Knol. 2008 Jul 28 , Creative Commons Attribution 3.0 License
Open Hemorrhoidectomy
In an open hemorrhoidectomy, hemorrhoidal tissue is excised in the same manner as in a closed procedure, but here the incision is left open. Surgeons may opt for open hemorrhoidectomy when the location or amount of disease makes wound closure difficult or the likelihood of postoperative infection high. Often, a combination of open and closed technique is utilized. Complications following open hemorrhoidectomy are similar to those that occur after closed hemorrhoidectomy.
Stapled Hemorrhoidectomy for Prolapsing Hemorrhoids
Stapled hemorrhoidectomy is the newest addition to the armamentarium of surgical internal hemorrhoid procedures. It has several aliases, including Longo's procedure, the procedure for prolapse and hemorrhoids (PPH, Ethicon Endo-surgery, Inc., Cincinnati, OH), stapled circumferential mucosectomy, and circular stapler hemorrhoidopexy.
Stapled hemorrhoidectomy is mostly used in patients with grade III and IV hemorrhoids and those who fail prior minimally invasive treatments. During stapled hemorrhoidectomy, a circular stapling device is used to excise a circumferential ring of excess hemorrhoid tissue, thereby lifting hemorrhoids back to their normal position within the anal canal.
Stapling also disrupts hemorrhoid blood supply. Studies have suggested that stapled hemorrhoidectomy results in less postoperative pain and shorter recovery compared with conventional surgery, but a higher rate of recurrence. Frequency of complications is similar to that following standard hemorrhoidectomy.
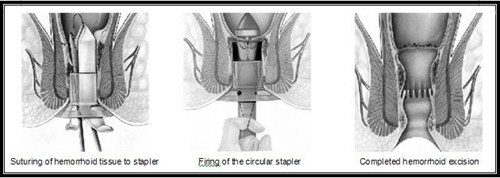
Stapled Hemorrhoidectomy (Procedure for Prapse and Hemorrhoids)
Source: Hemorrhoids:By Andrea C. Bafford, M.D. and Ronald Bleday, M.D [Internet]. Version 20. Knol. 2008 Jul 28 , Creative Commons Attribution 3.0 License
Rubber Band Ligation
A rubber band is placed around the base of the hemorrhoid inside the rectum. The band cuts off circulation, and the hemorrhoid withers away within a few days.
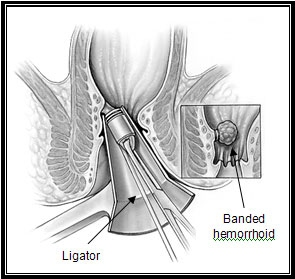
Rubber band ligation
Source: Hemorrhoids:By Andrea C. Bafford, M.D. and Ronald Bleday, M.D [Internet]. Version 20. Knol. 2008 Jul 28. Creative Commons Attribution 3.0 License
Lateral Internal Sphincterotomy
Lateral internal sphincterotomy or opening of the inner anal sphincter muscle is sometimes performed during hemorrhoidectomy in patients with high resting sphincter pressures. It is hypothesized to reduce postoperative pain. It is not used in most cases.


